Spermatogenesis sounds complex, but it is just how your body makes sperm. It happens inside the testicles. Early cells grow, divide, form tails, and turn into mature sperm. This process runs daily. If it slows or stops, natural fertility drops, even if testosterone levels are high. Hormones control each step. GnRH, FSH, LH, and testosterone tell the body when to start and when to slow down. Things like heat, illness, or testosterone replacement therapy can interfere with this process. Knowing how it works makes it easier to notice problems and talk to your doctor early.
Key Takeaways
- Spermatogenesis is how the testes make sperm, guided by GnRH, FSH, LH, and testosterone; when production slows, natural fertility typically declines.
- The process runs in stages—mitotic renewal, meiosis, then maturation—before epididymal finishing; one cycle takes roughly sixty-four to seventy-two days.
- Heat, smoking, obesity, illness, medications, and varicoceles can reduce sperm output; healthy diet, exercise, and cooler scrotal temperatures support quality.
- Testosterone replacement therapy often suppresses LH and FSH, dropping counts to very low or zero; recovery commonly occurs six to twelve months after stopping.
- Planning children while on TRT? Discuss hCG or SERM support, short-acting options, and regular semen analyses with clinicians to preserve fertility and adjust early.
Table of Contents
Understanding Spermatogenesis: A Simple Definition
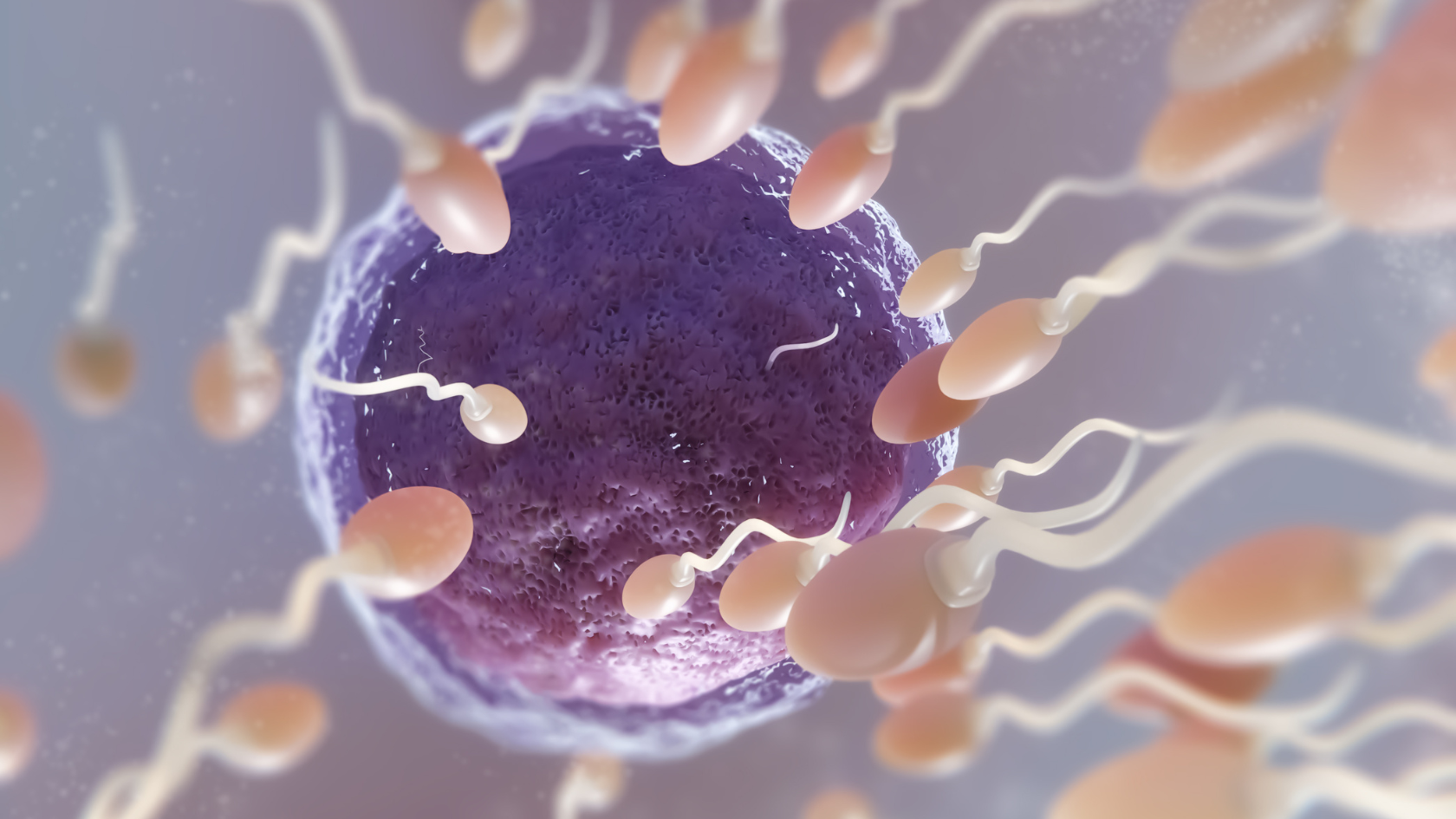
Spermatogenesis is how the body makes sperm. It starts at puberty and continues through most of life. It happens in three stages.
First, starter cells line the seminiferous tubules. They divide to keep the supply going. Some stay behind. Others move on to the next step. Second is meiosis. Each cell splits twice and ends up with half the usual DNA. This step matters because mistakes here can cause infertility or genetic issues. Third, round cells turn into mature sperm. They form heads and tails and lose extra material. Sertoli cells support them, and testosterone helps them grow. The sperm then move to the epididymis, where they learn to swim and can fertilize an egg.
The full process takes about 64 to 72 days. That means habits today affect sperm quality two months from now. The body makes millions of sperm every day, so small issues usually are not permanent. But heat, smoking, obesity, some medications, hormone problems, and varicoceles can lower output. Exercise, good food, and avoiding excess heat can help keep sperm healthy.
Spermatogenesis And Testosterone Replacement Therapy
Testosterone Replacement Therapy helps men with confirmed low testosterone. It can improve mood, muscle, and bone strength. But TRT tells your brain there’s enough testosterone, so it stops signaling your testes to make sperm. Your sperm count can drop to zero. Long-acting TRT like weekly shots or pellets keeps hormone levels steady.
This shuts down sperm production hard. Studies show up to 90% of men on these treatments have very low or no sperm within six months. Fertility usually comes back 6-12 months after stopping, but it can take longer if you’re older or already had testicular problems. Short-acting TRT like oral or nasal forms cause hormone spikes and dips.
Early research suggests these might keep some sperm production going. Ongoing trials are checking if oral testosterone can preserve fertility better. If you’re on TRT and want kids soon, talk to your doctor first. They might add hCG or SERMs to help keep your sperm production going during treatment. Some researchers are testing combinations that protect fertility while you’re on TRT.
The FDA is looking at making TRT easier to get, based on better safety data from December 2025. But easier access means doctors need to explain the fertility risks clearly. Everyone responds differently. Regular sperm tests and hormone checks help you see how your body is responding so you can adjust treatment early.
How Spermatogenesis Works and Why It Matters
Frequently Asked Questions
Not until very late in life. Production slows with age but usually continues, unlike egg production in women.
Roughly 64–72 days from stem cell to mature sperm. Add another 12–21 days for epididymal “finishing school.”
Permanent loss is rare. Most men regain sperm counts within a year after stopping TRT, especially if they start early fertility support.
Many have little proven benefit and some herbals may suppress LH/FSH. Always discuss supplements with your clinician first.
Maintain a healthy weight, quit smoking, limit alcohol, manage stress, and keep the testes cool (avoid tight heat-trapping clothing).
Repairing dilated scrotal veins often improves testicular temperature control, boosting sperm count and motility in many cases.
Hormone panels hint at testicular function, but only a semen analysis shows actual sperm output.
No. Women produce oocytes via oogenesis, a separate process that largely finishes before birth.
High core temperatures can temporarily lower sperm counts; most rebound within weeks once you recover.
FSH signals Sertoli cells to nurture developing sperm, ensuring proper growth and chromosomal division.